Gastric Bypass Surgery
Gastric bypass surgery is regarded as the gold standard procedure for the surgical treatment of severe obesity. It has been gradually refined over the past 30 years to produce a reliable, highly effective operation with a low risk of serious side effects.
In general the gastric bypass is a more forgiving procedure than a gastric band and is easier to live with.
The gastric bypass is regarded as gold standard not least because of its consistent and excellent results in achieving sustained weight loss and resolution of diabetes. The typical target is to lose about 70 – 80% of excess weight within two years. Most patients with type 2 diabetes who undergo a gastric bypass can expect to see a remarkable improvement in blood sugar control, often without the need for any regular diabetic medications. These results cannot be underestimated in terms of their transformative effects for patients, not only in terms of reduced illness and comorbidity but also because of the enormously positive impact it has on their physical and psychological well-being.
There are two types of gastric bypass, and your surgeon will discuss the best option with you.
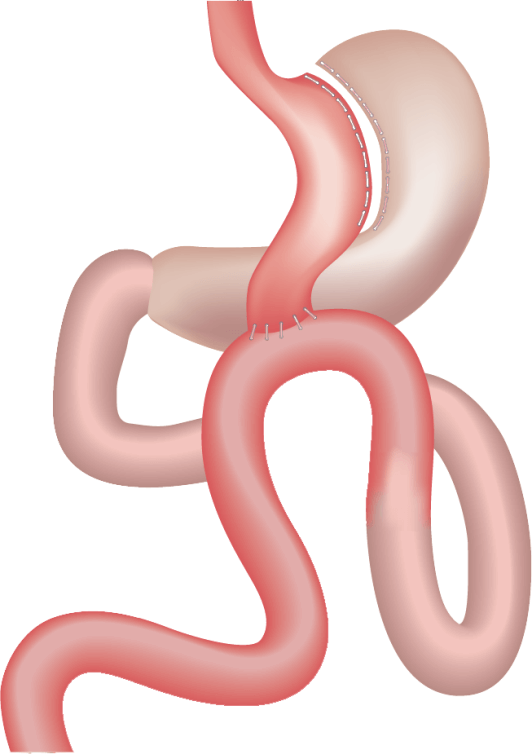
Roux-En-Y Gastric Bypass
This procedure is carried out laparoscopically (keyhole surgery) and uses special equipment to alter the way food flows through the intestines. First the stomach is turned into a small pouch, (about the size of a large egg). Next the small intestine is carefully measured, transected, and reattached onto the new stomach pouch. The pouch only allows smaller quantities of food into it and bypasses the rest of the stomach and the first metre or so of small intestine. The body reacts to this change by releasing large quantities of naturally occurring gut hormones after food, that suppress appetite and improve the way the body controls blood sugar levels. Whilst it is true that the gastric bypass does affect the absorption of food, this effect is really quite mild and so it is unusual for bypass patients to suffer with side effects of malabsorption such as diarrhoea or severe nutritional problems.
Careful follow-up is vital so that persistent vomiting or excessive weight loss (which may have a psychological component to it) are investigated and treated promptly. Blood tests need to be performed every three to four months and should include trace elements such as zinc, iron and magnesium, together with vitamin B12 and folate levels. Most bariatric patients are vitamin D depleted/deficient before they even have their surgery and so it’s our practice to also supplement this routinely as well.
A stricture (narrowing) of the newly created opening between stomach pouch and intestine is a fairly common problem in the early months after the procedure, but this is easily treated by stretching the narrowed area with a small balloon that is passed down a gastroscope (a flexible camera used to examine the stomach under sedation). Early surgical complications mirror those of the sleeve gastrectomy, including staple line leakage, bleeding and injury to other internal structures. All these complications can be minimised by ensuring the procedure is carried out by experienced surgeons with a good multi-disciplinary team. Later major problems are uncommon, but clinicians need to be aware of the increased risk of gallstones after rapid weight loss and unusual presentations of abdominal pain (often in the absence of vomiting) that might indicate the rare problem of an internal (Petersen’s) bowel hernia.
Dumping syndrome is worthy of a special mention as it is often referred to in a negative sense when gastric bypass is discussed. Dumping (which results from rapid emptying and absorption of sugars within the small bowel) is uniquely associated with the gastric bypass. As these high volumes of sugars are absorbed there is an over-exaggerated insulin response. This causes the blood sugar levels to fall rapidly and the patient experiences symptoms of hypoglycaemia (low blood sugar) such as anxiety, sweating, dizziness and fainting. It is often preceded by stomach cramps and diarrhoea, the net effect of which is to bring about a most helpful degree of wariness in the chocolate-loving bariatric patient.
One Anastomosis Gastric Bypass
The One Anastomosis Gastric Bypass (OAGB), also known as mini-gastric bypass is a minimally invasive procedure performed laparoscopically. During the OAGB procedure, the surgeon first reduces the size of the working stomach by creating a tube connected to the lower end of the gullet that is separate from the rest of the stomach. This tubular gastric pouch is then connected (anastomosed) to the small intestine, bypassing up to 200cm of the intestine that would otherwise be used to absorb food. This technique differs from the traditional Roux-En-Y Bypass (RYGB) which requires two connections (anastomoses).
OAGB typically results in loss of 30% to 40% of body weight (60-80% excess weight loss). The most rapid weight loss occurs in the first 6 months after surgery and then continues at a slower pace for up to another 18 months. This weight loss is achieved through restriction (the new gastric pouch can only hold a smaller quantity of food) malabsorption and most importantly by changing the levels of various natural gut hormones that are key to how the body controls appetite and the sensation of fullness. Substantial weight loss may lead to dramatic improvement, and even complete remission of many of the obesity-related medical problems. Long-term data shows that OAGB may result in a slightly better weight loss and resolution of diabetes than the RYGB.
The OAGB has few long term complications. Less than 5% of the patients may require revision surgery, with half of the revisional surgeries due to poor nutrition when longer lengths of small bowel are bypassed and the other half due to bile reflux, ulcer and/or weight regain.
One of the disadvantages of the OAGB include a greater likelihood that patients with OAGB will experience bile reflux than after a Roux-En-Y gastric bypass, which might affect their quality of life. The role of increased bile reflux as a possible risk factor for later development of gullet cancer is controversial. Another disadvantage of OAGB is a greater likelihood that the patient will develop significant vitamin and micronutrient deficiencies over time. Patients receiving OAGB must take regular vitamin and mineral supplements as instructed, and undergo lifelong, yearly monitoring.
For more detailed information on the complications and risks of Roux- en- Y gastric bypass, please click here and for one anastomosis (‘mini’) gastric bypass, click here.
Interested in beginning your weight loss journey? Fill in the contact form below or visit here to speak to our friendly team.


